Carotid Disease Management and Surgery for Stroke
Carotid disease, specifically carotid artery stenosis, refers to the narrowing of the carotid arteries, which are the major blood vessels in the neck that supply blood to the brain. Carotid artery stenosis is a significant risk factor for stroke, as it can lead to reduced blood flow to the brain and increase the likelihood of blood clots forming and traveling to the brain, causing a stroke.
Management of Carotid Disease:
- Lifestyle Modifications: Adopting a healthy lifestyle is crucial in managing carotid disease and reducing the risk of stroke. This includes quitting smoking, maintaining a healthy diet, engaging in regular physical activity, and controlling risk factors such as high blood pressure, diabetes, and high cholesterol levels.
- Medications: Medications may be prescribed to manage risk factors and reduce the risk of stroke. Common medications include antiplatelet agents (e.g., aspirin), anticoagulants (e.g., warfarin), blood pressure medications, cholesterol-lowering drugs (e.g., statins), and medications to control diabetes.
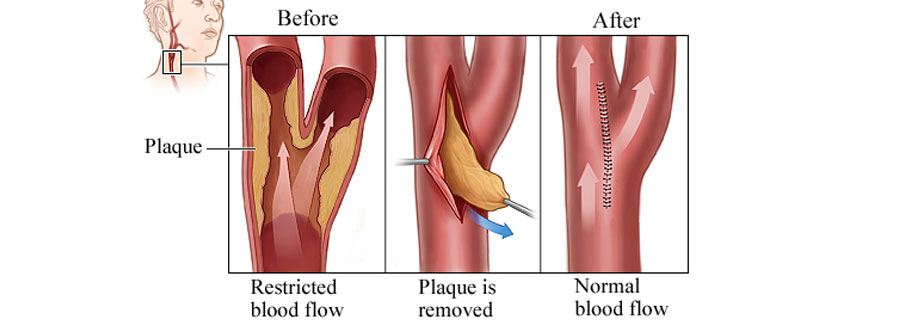
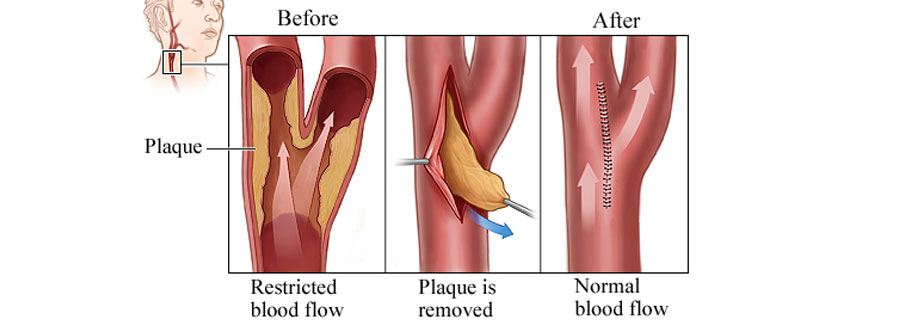
- Carotid Endarterectomy (CEA): Carotid endarterectomy is a surgical procedure performed to remove plaque and restore blood flow in the carotid artery. It is indicated for patients with significant carotid artery stenosis (usually above 70% narrowing) and who are at high risk for stroke. During the procedure, a vascular surgeon makes an incision in the neck, opens the affected carotid artery, removes the plaque, and then closes the artery with sutures.
- Carotid Artery Stenting (CAS): Carotid artery stenting is an alternative to CEA for treating carotid artery stenosis. It involves placing a stent (a mesh-like tube) in the narrowed segment of the artery to improve blood flow and prevent future strokes. CAS is generally considered for patients who are at higher risk for surgery or have certain anatomical characteristics that make CEA more challenging.